Holly Aitken, PhD received a fall 2025 microgrant from the Pediatric Orthopedic Society of North America (POSNA) for her project titled "Bone Remodeling and Contact Stress After Slipped Capital Femoral Epiphysis." This is a one-year project that will begin on December 1, 2025.
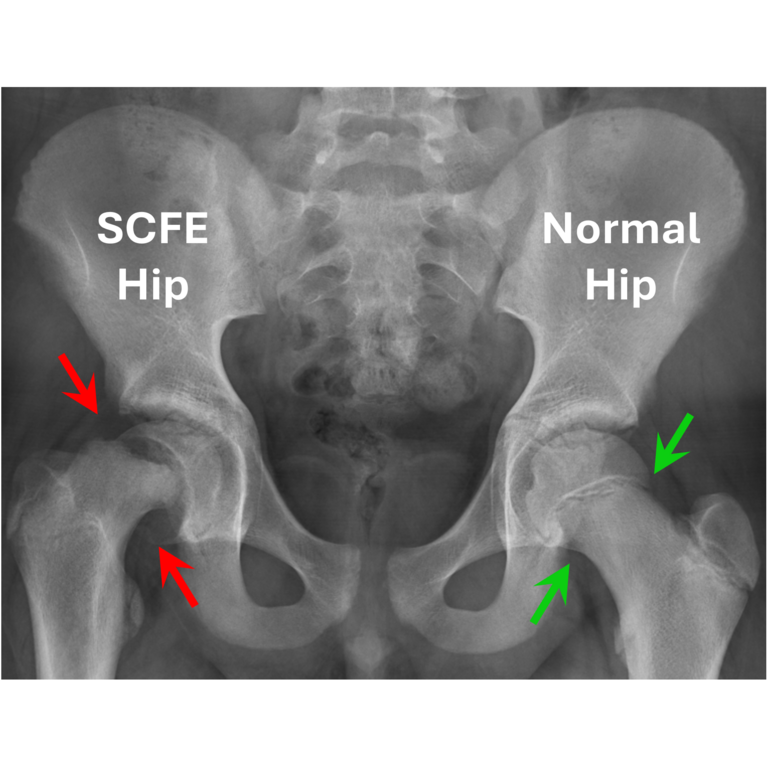
Slipped capital femoral epiphysis (SCFE) is a common disorder affecting adolescent patients in which the epiphysis separates from the metaphysis of the femoral neck. The proximal femoral epiphysis remains in the acetabulum, while the metaphysis rotates anteriorly, externally, and into extension. It can be a devastating injury with necrosis of the femoral head and rapid progression of hip arthritis even when managed urgently and appropriately. Multiple operative interventions have been proposed as possible management options, but these surgical interventions all impart modest morbidity and have shown variable outcomes depending on timing and the type of intervention. Some of the more conservative approaches, such as in-situ pinning, stabilize the hip from further changes in shape, but at the same time make permanent the changes in shape that have occurred to date. This permanently alters the mechanics of the hip and can create extra-articular impingement and intra-articular contact stress elevations, both of which are concerning for premature osteoarthritis development. Bony remodeling of the pinned hip is expected given its skeletal immaturity, but the extent of that remodeling is unpredictable and governs the need for additional surgical procedures to minimize future osteoarthritis risk.
This study aims to quantify bone remodeling approximately 5 years after in-situ pinning of the post-SCFE hip and any associated changes in hip contact stress. Identifying how post-SCFE hips remodel and change contact mechanics would provide guidance for surgeons regarding when to intervene with secondary procedures needed to correct residual or remodeled deformity.
To achieve this aim, new research-specific pelvis CT scans of individuals approximately 5 years after development of a SCFE deformity will be collected, from which patient-specific bony geometry can be obtained to create 3D SCFE hip-specific models. From these models, contact stresses will be computed using a validated discrete element analysis (DEA) methodology, and 3D coverage angles around the acetabulum and regional joint sphericity/congruity will be calculated. The contact stress and coverage/congruity data will then be compared to contact stresses and coverage/congruity measures obtained from 3D hip models created from each patient’s existing clinical imaging that was acquired at the time of initial SCFE deformity. It is anticipated that hip joints that remodel towards a more spherical joint articulation will have decreased contact stress after 5 years. Data generated by this pilot project will be used to design a statistically powered investigation of common remodeling patterns and their correlations to contact stresses.